Myth's About Snoring
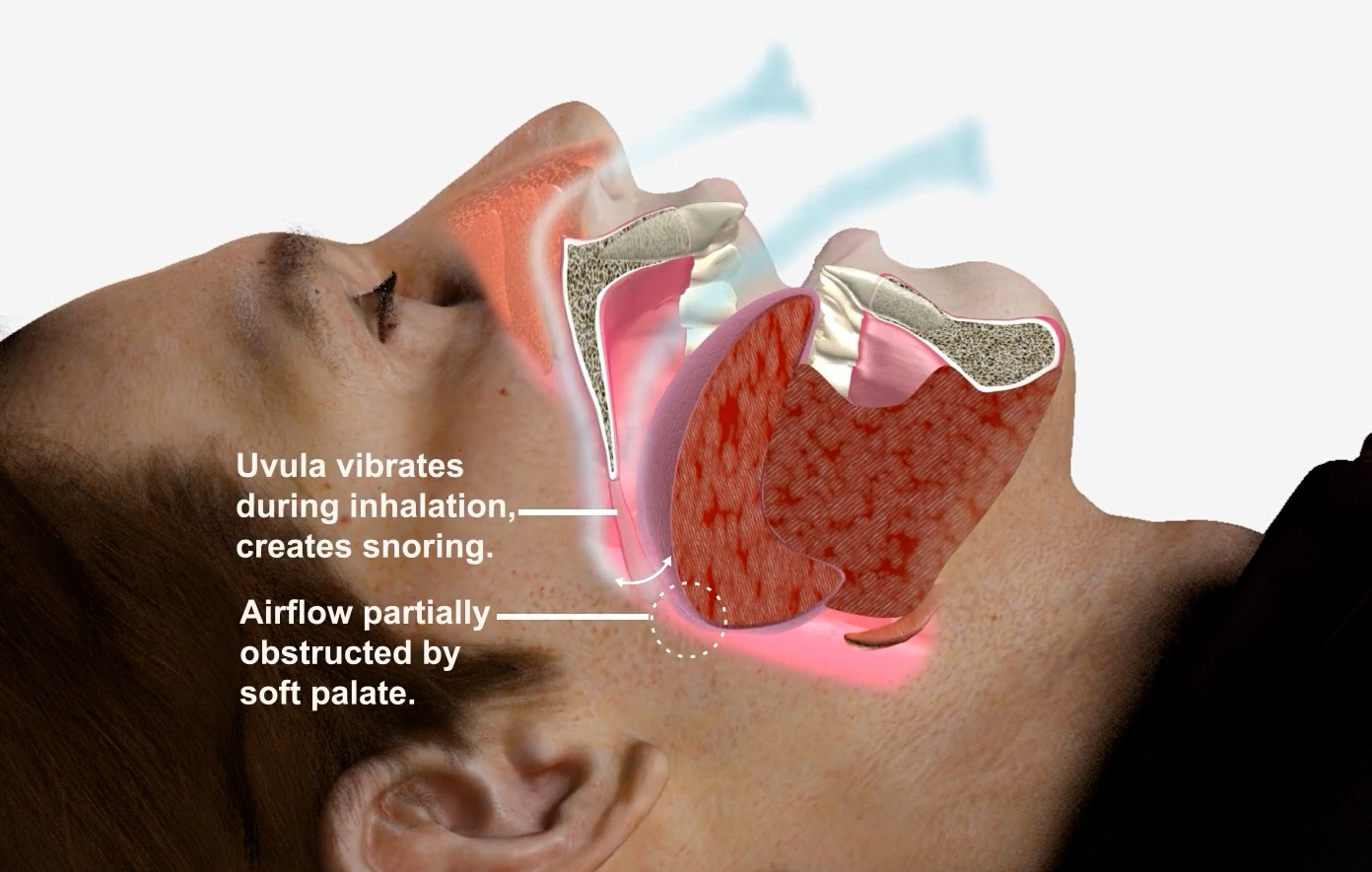
Snoring is the hoarse or harsh sound that occurs when air flows past relaxed tissues in your throat, causing the tissues to vibrate as you breathe. Nearly everyone snores now and then, but for some people it can be a chronic problem. Sometimes it may also indicate a serious health condition. In addition, snoring can be a nuisance to your partner. Lifestyle changes, such as losing weight, avoiding alcohol close to bedtime or sleeping on your side, can help stop snoring. In addition, medical devices and surgery are available that may reduce disruptive snoring. However, these aren’t suitable or necessary for everyone who snores.
- Snoring is harmless and just a nuisance. Fact: While occasional snoring may be harmless, frequent or loud snoring can be a sign of obstructive sleep apnea (OSA), a serious sleep disorder that affects breathing during sleep. Left untreated, OSA can lead to high blood pressure, heart disease, stroke, and other health problems.
- Only overweight people suffer from OSA. Fact: While being overweight increases the risk of OSA, anyone, including people of average weight or children, can develop the condition. Factors like the shape of your airway, family history, or age can also contribute to OSA.
- Snoring always indicates OSA. Fact: Not all snorers have sleep apnea. Snoring without pauses in breathing may not be related to OSA, but it’s essential to watch for symptoms like gasping for air during sleep, excessive daytime sleepiness, or difficulty concentrating, which may signal a sleep disorder.
- Drinking alcohol helps reduce snoring. Fact: Alcohol relaxes the muscles in the throat, which can actually make snoring and OSA worse. Drinking before bed may increase the severity and frequency of snoring by causing airway obstruction.
- CPAP is the only treatment for OSA. Fact: While Continuous Positive Airway Pressure (CPAP) therapy is a common and effective treatment, it is not the only option. Other treatments, such as oral appliances, weight management, positional therapy, and, in some cases, surgery, can also help manage OSA.
- Snoring and OSA only affect men. Fact: Though OSA is more common in men, women can also suffer from this condition. In fact, postmenopausal women have a higher risk of developing OSA. Symptoms in women can sometimes be subtler, leading to under diagnosis.
- Kids don't suffer from sleep apnea. Fact: Children can develop obstructive sleep apnea, often due to enlarged tonsils or adenoids. Symptoms in children may include restless sleep, bedwetting, behavioral issues, or hyperactivity, which are sometimes mistaken for other conditions like ADHD.
- If you don’t feel tired during the day, you don’t have OSA. Fact: While excessive daytime sleepiness is a common symptom of OSA, not everyone experiences it. Some people with OSA may feel fine during the day but still face serious health risks from untreated apnea, such as cardiovascular issues or cognitive impairment.
- Surgery is a quick fix for snoring and OSA. Fact: Surgery is not a guaranteed cure for snoring or OSA and is typically considered after other treatments have been tried. Many patients find greater long-term success with non-surgical treatments, such as CPAP or oral appliances.
- OSA isn’t dangerous—it’s just about sleep. Fact: OSA is a serious medical condition that goes beyond sleep. Untreated OSA increases the risk of high blood pressure, heart attacks, strokes, diabetes, and even sudden death. It can also affect quality of life, leading to impaired concentration and memory, mood swings, and a higher likelihood of accidents.
- Daytime fatigue is just due to poor sleep habits, not a medical condition.Fact: Persistent daytime fatigue can indicate OSA, especially if it’s accompanied by other symptoms like difficulty concentrating, memory issues, or mood changes.
- Snoring and OSA aren’t affected by your sleep position.Fact: Sleep position can actually make a world of difference! For many people with snoring or OSA, lying on their back can make symptoms worse, as gravity pulls the tongue and soft tissues backward, blocking the airway. Sleeping on your side, however, can help keep the airway open, often reducing both snoring and OSA symptoms. A simple shift in position might lead to quieter, more restful nights!
Snoring and relation to OSA
Snoring is often associated with a sleep disorder called obstructive sleep apnea (OSA). Not all snorers have OSA, but if snoring is accompanied by any of the following symptoms, it may be an indication to see a doctor for further evaluation for OSA:
- Witnessed breathing pauses during sleep
- Excessive daytime sleepiness
- Difficulty concentrating
- Morning headaches
- Sore throat upon awakening
- Restless sleep
- Gasping or choking at night
- High blood pressure
- Chest pain at night
- Your snoring is so loud it’s disrupting your partner’s sleep
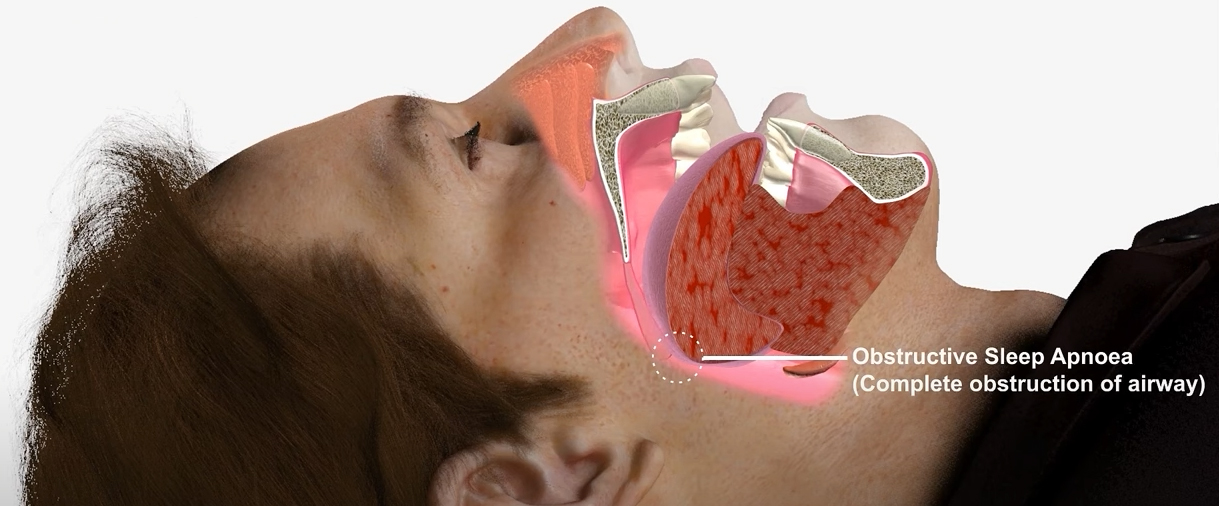
In children, poor attention span, behavioral issues or poor performance in school OSA is often characterized by loud snoring followed by periods of silence when breathing stops or nearly stops. Eventually, this reduction or pause in breathing may signal a person to wake up, and they may awaken with a loud snort or gasping sound. They may sleep lightly due to disrupted sleep. This pattern of breathing pauses may be repeated many times during the night. People with obstructive sleep apnea usually experience periods when breathing slows or stops at least five times during every hour of sleep.



What is Obstructive Sleep Apnea
Obstructive Sleep Apnea (OSA) is a common and serious sleep disorder in which a person’s breathing is repeatedly interrupted during sleep due to a blockage or narrowing of the airway. This obstruction is typically caused by the relaxation of the muscles in the throat, which can cause the airway to collapse, blocking airflow. When this happens, the person temporarily stops breathing (apnea), leading to reduced oxygen levels in the blood and causing the person to briefly wake up to resume breathing.

How to objectively diagnose OSA ?
Polysomnography (PSG)
The gold standard for diagnosing OSA, this overnight sleep study provides detailed measurements of brain activity, breathing patterns, oxygen levels, and heart rate. Objective Data: It calculates the Apnea-Hypopnea Index (AHI), which is the average number of apneas (pauses in breathing) and hypopneas (shallow breathing) per hour of sleep.
Severity classification based on AHI:
Mild: AHI 5-15 events/hour
Moderate: AHI 15-30 events/hour
Severe: AHI > 30 events/hour
Home Sleep Apnea Testing (HSAT)
Portable monitors used at home measure airflow, respiratory effort, and blood oxygen saturation (SpO2).
Provides an AHI, similar to PSG but with fewer measured parameters.
Adjunct techniques: Peripheral Arterial Tonometry (PAT) Oximetry, Actigraphy, Upper Airway Imaging, Drug Induced Sleep Endoscopy (DISE).

Oral Appliance therapy in OSA
Oral appliance therapy (OAT) is a proven option for treating mild to moderate obstructive sleep apnea (OSA) and can be an effective alternative to CPAP for many patients. Custom-made advanced devices like the DreamVent comfortably move the lower jaw forward, helping to keep the airway open. With an integrated airway channel, DreamVent can bypass nasal congestion and prevent airway collapse from the tongue, soft palate, and lateral walls—offering a convenient, comfortable choice for those seeking relief from OSA symptoms.

Treatment Options in OSA
1. Positive Airway Pressure (PAP) Therapy:
- Continuous Positive Airway Pressure (CPAP): Delivers a continuous stream of air to keep the airway open during sleep.
- Bi-Level Positive Airway Pressure (BiPAP): Provides two levels of pressure: a higher pressure during inhalation and a lower pressure during exhalation.
- Auto-Titrating Positive Airway Pressure (APAP): Adjusts the pressure automatically based on the patient’s needs throughout the night.

2. Lifestyle Modifications:
- Weight Loss: Reducing excess weight can significantly decrease the severity of OSA.
- Positional Therapy: Encouraging patients to avoid sleeping on their back can reduce airway collapse.
- Avoiding Alcohol and Sedatives: These substances can relax the throat muscles and worsen OSA.

- Nasal Septoplasty: A surgical procedure to straighten the nasal septum, the wall between the nostrils, to improve airflow.
- Adenotonsillectomy: Removal of the adenoids and tonsils, often to alleviate breathing issues or recurrent infections.
- Uvulopalatoplasty: Surgery to reshape or remove part of the uvula and soft palate to open up the airway.
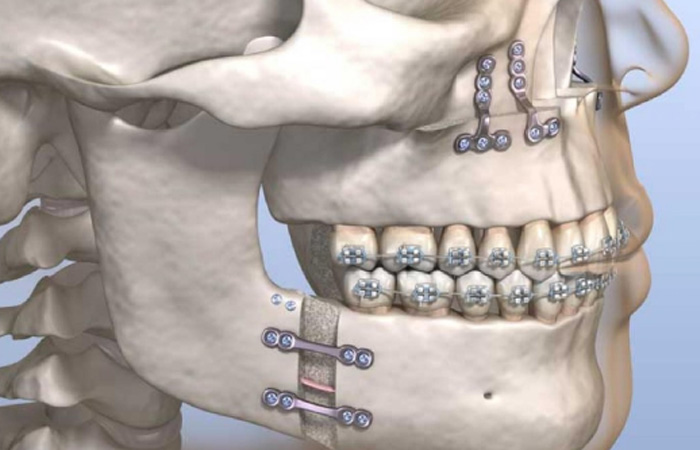
- Maxillomandibular Advancement: Moving the upper (maxilla) and lower (mandible) jaws forward to enlarge the airway space.
- Genioglossus Advancement: A procedure to reposition the genioglossus (tongue) muscle, pulling it forward to prevent airway collapse.
- Hyoid Suspension: Securing the hyoid bone in the neck to a more forward position to help keep the airway open during sleep.
- Bariatric Surgery: Bariatric surgery involves surgical procedures designed to limit food intake or reduce nutrient absorption to promote weight loss, thereby addressing the problem of OSA.
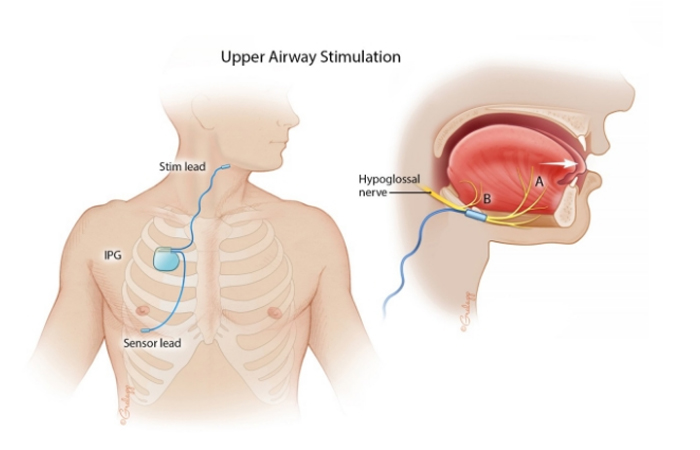
Hypoglossal nerve stimulation is a treatment for obstructive sleep apnea (OSA) that activates the hypoglossal nerve to keep the airway open during sleep.
Source: Stanford Medicine, otolaryngology- Head & Neck Surgery
3. Nasal Surgery
- Septoplasty: Corrects a deviated nasal septum to improve nasal airflow.
- Rhinoplasty: May be performed to address structural abnormalities in the nose that contribute to obstructed airflow.
- Turbinoplasty: Reduces the size of the nasal turbinates to enhance airflow.

4. Throat Surgery:
- Uvulopalatopharyngoplasty (UPPP): Removes excess tissue from the throat (uvula, soft palate, and possibly tonsils) to widen the airway.
- Tonsillectomy: Removal of enlarged tonsils that may obstruct the airway.
- Adenoidectomy: Removal of the adenoids, which can block the airway in some patients.

